Warning Signs of Diabetes and Symptoms of Hyperglycemia
Source: Pixabay
Diabetes mellitus encompasses a group of metabolic diseases characterized by hyperglycemia (increased blood sugar levels) due to abnormalities in the secretion and/or action of insulin.
There are different types of diabetes, mainly Type 1 diabetes (which is commonly diagnosed in childhood), Type 2 diabetes and Gestational Diabetes (Caused in pregnancy).
The prevalence of diabetes has increased considerably in recent years, to the extent that there are currently 246 million patients with diabetes in the world. According to various health organizations, it is estimated that this number will double in 2030.
Type 2 diabetes is one of the chronic diseases that most affects the elderly. Half of people with diabetes are over 60 years old. Prevalence estimates for people age 60 and older range from 15% to 20%, with the highest rates associated with people age 75 and older.
Diabetes mellitus is a disease that does not usually cause many symptoms in the early stages, which is why it has been called the "silent" disease. In fact, on many occasions, the diagnosis of the disease is made when there are already complications such as diabetic retinopathy, chronic kidney disease, peripheral artery disease, peripheral neuropathy, etc.
In the older adult, diabetes not only reduces life expectancy, but it is also one of the main causes of functional deterioration and dependency.
Epidemiological Data for Diabetes
Diabetes is the leading cause of chronic kidney failure. A diabetic patient is 20 times more likely to develop kidney failure than a non-diabetic person.
Diabetes is the main cause of acquired blindness in patients of productive age. A diabetic patient is 4 times more likely to be blind than a non-diabetic patient.
A patient with diabetes is 4 to 6 times more likely to have a stroke or cerebral hemorrhage.
A diabetic patient is 4 times more likely to have a myocardial infarction.
Although this is one of the few diseases that most affects the female sex, on average men with diabetes die at a younger age than women (67 vs. 70 years respectively), and only 20% of men who have developed this disease live more than 75 years.
The World Health Organization (WHO) calculates that in 2018 the direct and indirect healthcare costs associated with this disease were around 548 billion dollars worldwide.
Know Your Risk
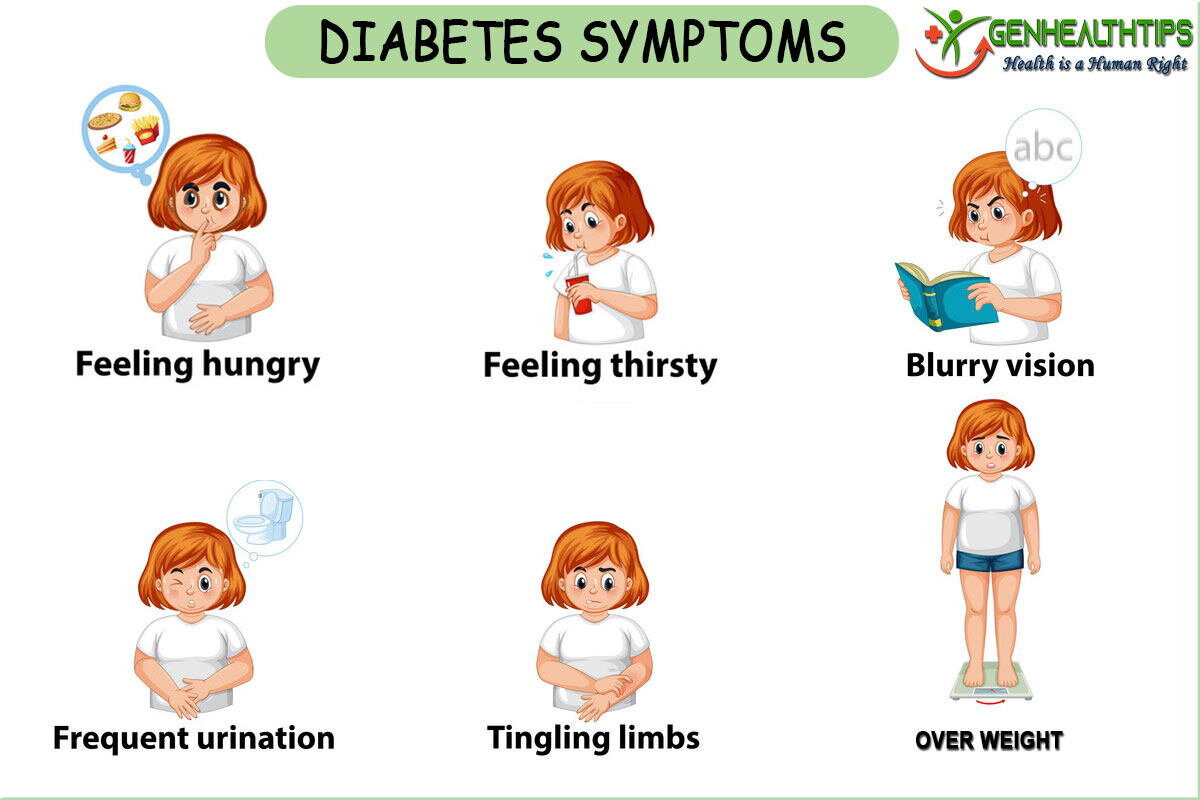
Signs and Symptoms of Diabetes Mellitus
The symptoms of diabetes mellitus are caused by a chronic hyperglycemic state that leads to disturbances in the functioning of various organs and systems. The main warning signs that can guide the diagnosis of diabetes mellitus are listed below:
Frequent infections that do not heal easily.
Thirst (polydipsia).
Frequent urination (polyuria).
Extreme hunger (polyphagia) associated with weight loss.
Blurry vision.
Nausea and vomiting.
Extreme tiredness and weakness.
Muscle cramps
Irritability and changes in mood.
Dry and itchy skin.
Tingling, pain, or loss of feeling in the hands and/or feet.
It is important to note that each person may experience symptoms in a different way, even some people with diabetes have no symptoms. The symptoms can be mild and almost imperceptible and are easy to confuse with the signs of aging, in fact, half of Americans with diabetes don't know it.
Source: GENHEALTHTIPS
Diabetes Diagnosis
The diagnosis of diabetes mellitus is based on the determination of blood sugar levels. Below are the criteria established by the United States Diabetes Association (ADA) and WHO for the diagnosis of this disease.
Plasma glucose values ≥ 126 mg / dL obtained after 8 hours of fasting, or ≥ 200mg / dL at any time of the day associated with the presence of cardinal symptoms (polyuria, polydipsia, and unexplained weight loss), these results must be confirmed twice before establishing the diagnosis. In contrast, the finding of plasma glycemia ≥ 200 mg / dL in a single oral glucose tolerance test is sufficient to reach a definitive diagnosis. (The oral glucose tolerance test consists of plasma glucose measured 2 hours after ingestion of 75g of glucose in 300 mL of water administered after an overnight fast.) Glycated hemoglobin greater than 6.5%
Depending on the diagnostic criteria established by the WHO and the ADA, the following diagnostic categories can be followed:
Normoglycemia: Fasting blood glucose <110 mg/dL and Oral glucose tolerance test (PTG) <140 mg/dL.
Impaired Fasting Blood Glucose (GAA): Fasting blood glucose = 110-125 mg / dL.
Oral Glucose Intolerance (IGT): Fasting blood glucose <126 mg / dL and Oral Glucose Tolerance Test (PTG) = 140-199 mg / dL.
Diabetes: Fasting blood glucose ≥ 126 mg / dL or Blood glucose taken at any time of the day ≥ 200mg/dL in the presence of cardinal symptoms (polyuria, polydipsia, and unexplained weight loss) or Oral glucose tolerance test (PTG) ≥ 200 mg / dL. Glycated hemoglobin greater than 6.5%
What is Glucose Intolerance?
Glucose intolerance is considered a prediabetic state, blood glucose levels are higher than normal but not high enough to be included in the definition of diabetes. However, many people with glucose intolerance develop type 2 diabetes in less than 10 years, according to studies by the Department of Endocrinology at the National Institute of Nutrition. Glucose intolerance also increases the risk of stroke and stroke. People with prediabetes can prevent the development of the disease by establishing a balanced diet and exercising regularly.
Source: Pixabay
Complications of Diabetes
The consequences of diabetes can be serious:
Cardiovascular:
Higher cardiovascular morbidity and mortality rate
Amputations: due to neuropathy, poor wound healing, and peripheral vascular insufficiency.
Increased incidence of ischemic heart disease and congestive heart failure (diabetic cardiomyopathy).
Increased incidence of cerebrovascular diseases, usually ischemic strokes.
Ophthalmic: the most frequent cause of blindness in the elderly is diabetic retinopathy, whose evolution depends on the duration of the disease and the degree of glycemic control. Cataract development is also common.
Neurological: hyperosmolar coma, dementia, cognitive decline, and depression; peripheral neuropathies: sensory deficit, neuropathic pain, autonomic dysfunctions.
Renal: kidney failure and urinary sepsis.
Gastrointestinal: gastroparesis and disorders in the motility of the large and small intestines.
Osteomuscular: older adults with diabetes are at increased risk of hip fracture.
Sexual dysfunction: in both men and women.
Functional deterioration and worse quality of life.
Know Your Risk
Associations of Cancer to Diabetes
Elevated cholesterol and insulin levels show a positive association with the development of cancers of the liver, pancreas, colon and rectum, bladder, as well as prostate. It’s a key factor contributing to the metabolic syndrome as well as endovascular/inflammatory response elevation, contributing to growth hormone, insulin and thrombosis dysregulation. A modest increase in risk is observed for these cancers estimated to be ~ 20%.
Furthermore, diabetes is strongly associated with an elevated body mass index (BMI). We do know that fat is not equally distributed around the body, but rather accumulates subcutaneously in certain parts of the body such as the abdomen. Intra-abdominal fat stores may be a better predictor of chronic disease risk than overall body fatness.
The evidence is convincing that greater body fatness increases the risk of cancers of the esophagus (adenocarcinoma), colon and rectum, pancreas, and kidney.
For every 5 kg/m2 increase in BMI within the range considered “normal” and above (which is where you fall in), risk increases by 50%–55% for esophageal adenocarcinoma, roughly 30% for kidney cancer, and 10%–15% for colorectal, and pancreatic cancer.
Treatment for Diabetes
Source: Pixabay
Specific treatment for type 2 diabetes will be determined by your doctor based on the following:
Your age, general health, and medical history.
The stage in which the disease is found.
Your tolerance for certain medications, procedures, or therapies.
Your expectations for sickness evolution. Your opinion and preferences.
The goal of treatment is to keep blood glucose levels as close to normal as possible. Control of blood glucose levels are given importance through the monitoring of levels, regular physical activity, a meal plan, and routine health care. Diabetes treatment is a constant process of monitoring and education that includes not only the person who has diabetes, but also health professionals and family members of the patient.
Type 2 diabetes can often be managed through weight loss, improved nutrition, and regular exercise. However, in some cases, these measures are not enough and oral medications and insulin must be used. Treatment frequently includes the following:
Diet low in simple sugars, and rich in complex fiber.
Plant-based diet.
Weight control.
Regular aerobic and core exercise programs.
Regular foot inspections.
Oral medications and insulin replacement therapy, as directed by your doctor.
Regular monitoring of glycated hemoglobin levels.
The glycosylated hemoglobin test is very useful since it allows to determine the average of glucose levels in the blood in the last three months. This test helps establish whether the patient was in control during this time. It is recommended that this test be performed at least twice a year if the results are normal, and more often if the blood glucose levels are not as desired.
Untreated or inappropriately-treated diabetes can cause kidney, leg, foot, eye, heart, nerve and blood circulation problems, which can lead to kidney failure, gangrene, amputation, blindness, or stroke. Therefore, it is important to follow a strict treatment plan.
Studies carried out on diabetes have made it possible to establish more effective control methods and treatments. Other methods of insulin delivery using inhalers and pills are currently being studied. Pancreas transplantation is also underway.
Sources
1. Rubin RJ. Health care expenditures for people with diabetes mellitus. J Clin Endocrinol and Metabol 1994; 78: 809 A-809 E.
2. American Diabetes Association. Clinical Practice Recommendations 2015. Diabetes Care 2015; 27(Suppl 1): s1-150.
3. The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine; 329: 977-86.
4. Morley JE, Kaiser FE. Unique aspects of Diabetes Mellitus in the elderly. Clin Geriatr Med 1990; 6(4):693-702.
5. Davidson MB. How do we diagnosis diabetes and measure blood glucose control? View 11 (diagnosing) a clinical bases for the diagnosis of diabetes. Diabetes spectrum 2001; 14: 67-70.
6. American Diabetes Assoc. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2004; 22 (Suppl 1): S15-S35.